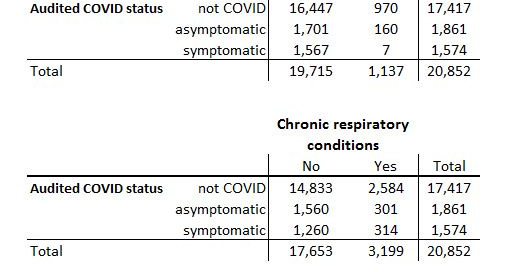
In my previous post in this series we observed 1,574 out of 3,435 (45.8%) adult in-hospital deaths meeting the criteria we might adopt for symptomatic COVID death; that is to say they not only tested positive prior to death but were suffering from an acute respiratory condition. It follows that we may classify the remaining 1,861 as asymptomatic COVID (testing positive with no acute respiratory condition) and bake a few crosstabulations again to see how things stack up.
The top section of the attached table provides a crosstabulation of adult in-hospital deaths over the period Feb ’20 – Sep ’21 involving non-COVID pneumonia (bacterial and viral, including influenza) and our newly established audited COVID status indicator. We find 11 asymptomatic COVID deaths associated with non-COVID pneumonia (18.0%) which suggests diagnostic tests indicated positive for both. The waters muddy further when we discover 15 symptomatic COVID deaths that are also associated with non-COVID pneumonia (24.6…