In the primary post for this analysis our eyeballing of a colourful slide provided two conclusions:
That there is no difference in the distribution of comorbidities for COVID-19 deaths during 2020-21 and influenza deaths during 2017-19;
That there is no difference in the distribution of comorbidities for COVID-19 deaths pre and post vaccination rollout.
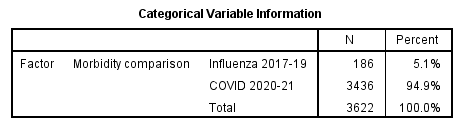
Eyes are one thing but rigorous hypothesis testing another, so let us run the data through generalised linear modelling (GLM) with the parametric distribution set to Tweedie with identity link and parameter estimation based on Fisher’s method using maximum likelihood as the scale parameter. This sounds complicated but this is just a fancy way of conducting plain old analysis of variance for a variable - count of diagnoses made - that is ostensibly non-Normal. Herewith key outputs…