Emergency Department Admissions: Analysis of CDS Dataset (part 6)
I analyse an anonymised data dump of 1.9 million admissions records to the emergency departments of an undisclosed NHS Trust for the period June 2017 – September 2021
Death is a big deal, especially if folk die in the emergency department, so I’m going to take a closer look at this outcome for the pre-pandemic period of January 2017 – February 2020 and then extend the analysis to consider all deaths through to September 2021.
Here’s what the multilayer perceptron neural network model for the prediction of deaths in A&E churned out in terms of variable importance:
This makes a lot of sense and matches my own experience of nine years of working between cardiology, cardiac surgery and A&E in a busy teaching hospital. Death-wise we’re talking about an elderly intake with multiple illnesses and likely suffering a cardiac condition requiring treatment, and arriving by ambulance (no doubt under a category 1 call). The cardiac procedure in question is almost certainly going to be thrombolysis, though defibrillation will also feature if paramedics were unable to secure some sort of stability.
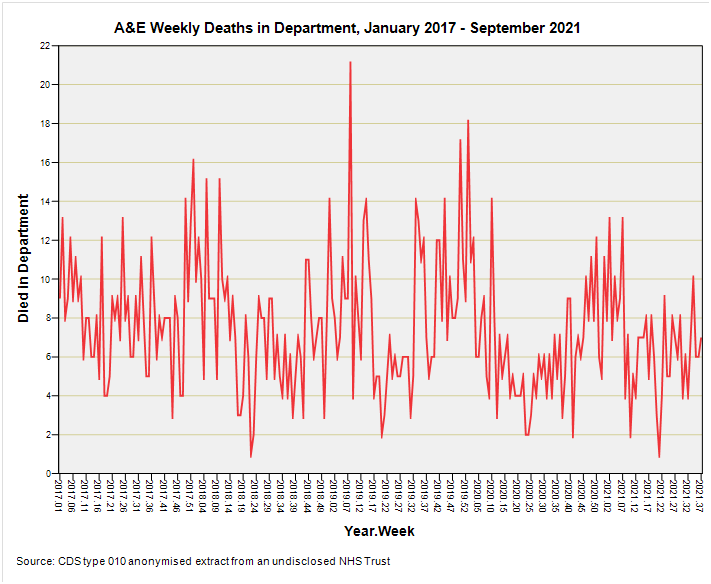
So let’s have a look at deaths in the department each week for the period 2017/w1 – 2021/w37:
Can anybody spot the pandemic? Me neither.
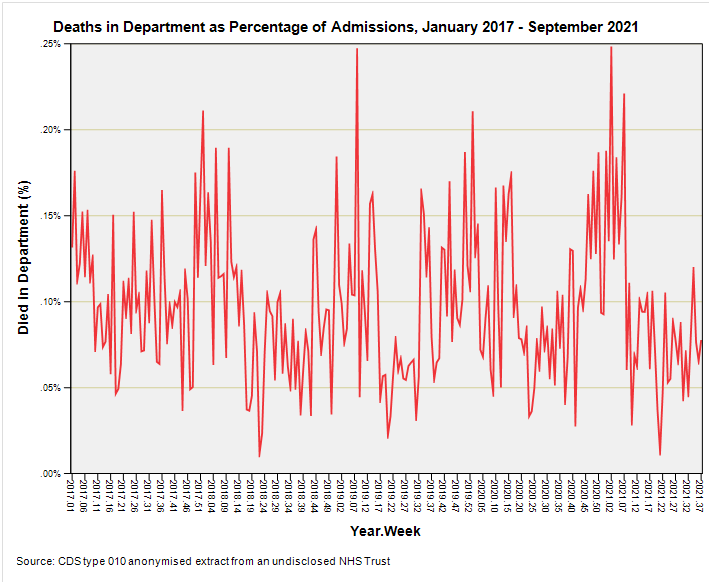
OK, so we know that A&E admissions fell through the floor as doors were closed so how about we calculate the percentage of deaths in the department in relation to total admissions to try and flatten the pitch that way? Sounds like a good idea? Then try this for size:
The pandemic of a ‘novel and deadly’ virus still doesn’t appear in spring of 2020 as it should, according to the narrative that was spun, and all we see is more of the same variation in the rate of departmental death from January 2017 right through to September 2021.
We might say it was business as usual when it came to death, yet the government had us quaking in our boots (some rather unpleasant senior NHS suits also, I might add).
So if people coming in on a blue light weren’t dying in accordance with the novel and deadly narrative then who was?
In-hospital Death
I’m now going to drop a couple of slides to get people thinking the unthinkable.
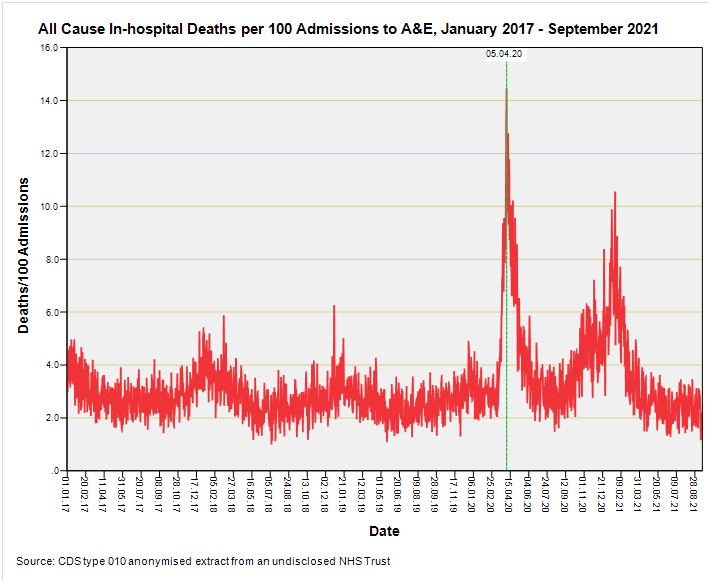
These are simple slides and they could be produced by every single band 6 Information Officer in every NHS Trust in the land, for all I am going to do is count the number of admissions to A&E on a daily basis then count the number of all cause in-hospital deaths on a daily basis. I’ll present this information on a dual axis plot for the period January 2020 – September 2021, and then I’ll derive a rate that is daily all cause in-hospital deaths per 100 Admissions to A&E for the period January 2017 – September 2021 and present this in a second slide. Here we go…
Readers should have got the jist of this in more or less the same manner as being hit round the head by a 4 x 2 of seasoned pine or punched in the face by Mike Tyson; it being one of those delicate little points like that.
We can now see that most of the dying in this NHS Trust was done when A&E admissions were a fraction of former levels and doors were closed, yet the narrative we were sold by the government and media is that a novel and deadly virus that was rampaging through the population had people being ferried to hospital by ambulance in droves.
This was clearly not the case for, in this Trust at least, A&E intake dropped to just ~38% of typical activity levels after which in-patients started dying.
The second slide makes this point in a somewhat subtle manner, for if ambulances were ferrying large numbers of COVID-stricken folk in for treatment as presented to us by the media then the death rate would fall to an all-time low. Except that it peaked, and pointedly so.
What Happened To Clinical Governance?
Simple audits of casenotes with presentation at regular monthly mortality and morbidity meetings should have cleared these matters up at the time, but I doubt if such searching discussions ever took place as they should have done. I’m betting that nobody questioned the deaths and nobody questioned the protocols and polices. This is ironic because each NHS Trust dealing in acute medicine will possess a team of band 4 - 6 Clinical Audit Facilitators managed by a Head of Clinical Audit as part of the Clinical Governance framework. Just when we needed it most Clinical Governance failed the nation.
Kettle On!




Could A&E admissions be a bad proxy for hospital admissions? By that I mean only sickest come in, so the hospital admission rate could be high, thereby putting demand on hospital beds, but not A&E. Pretty sure we've been there already, but just another devil's advocate.
Hi John, may I request again that you include a short summary of your conclusions at the beginning of each essay?