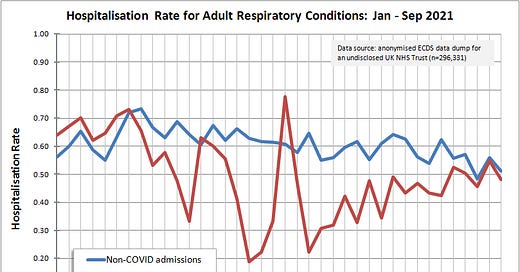
Hospitalisation Rate For Adult Respiratory Conditions (part 1)
Lessons from an undisclosed NHS Trust
Sometimes statisticians overlook what is plain and simple and sitting right under our noses. Today I am going to wrap split-file propensity-adjusted staged multivariate logistic regression in Clingfilm and put it back in the pantry. My stats package will be put in Tupperware and we’ll take out a fresh tub of Excel and spread it nice and simple.
We shall consider all adult (18y – 99y) admissions to the emergency department who were diagnosed with either an acute (e.g. pneumonia) or chronic (e.g. asthma) respiratory illness. We shall divide them in to those who were discharged directly back home and those who were given a bed in a short stay ward, general ward, CCU, HDU or ICU (i.e. hospitalised). We shall take a note of whether they tested positive for COVID-19 and we shall take a note of their vaccination status (unvaccinated at admission; dose 1 received prior to admission; dose 2 received prior to admission). We shall not deceive people by messing around with definitions: unvaccinate…