Underlying Cause Of Death (part 2)
Investigation of the hike in care home non-COVID deaths in England & Wales during 2020 (rev 1.0)
In my previous newsletter we discovered a hike in pneumonia cases coinciding with the hike in care home deaths in England over the period 2020/w13 - 2020/w21. Does this explain everything we need to know?
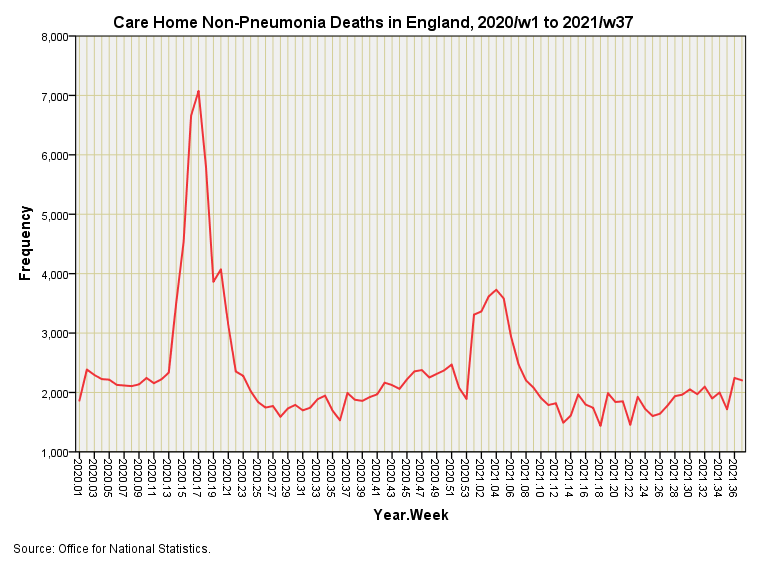
We may find the answer by subtracting weekly pneumonia care home deaths for England from weekly all cause care home deaths and squinting at the resultant time series:
I’ll take that as a resounding ‘no’, then! Thus, when those certifying physicians declared that hike in non-COVID deaths during early 2020 they weren’t getting confused, neither were they being distracted by PCR test results. These were not miscoded respiratory deaths as some are suggesting, they were something else entirely.
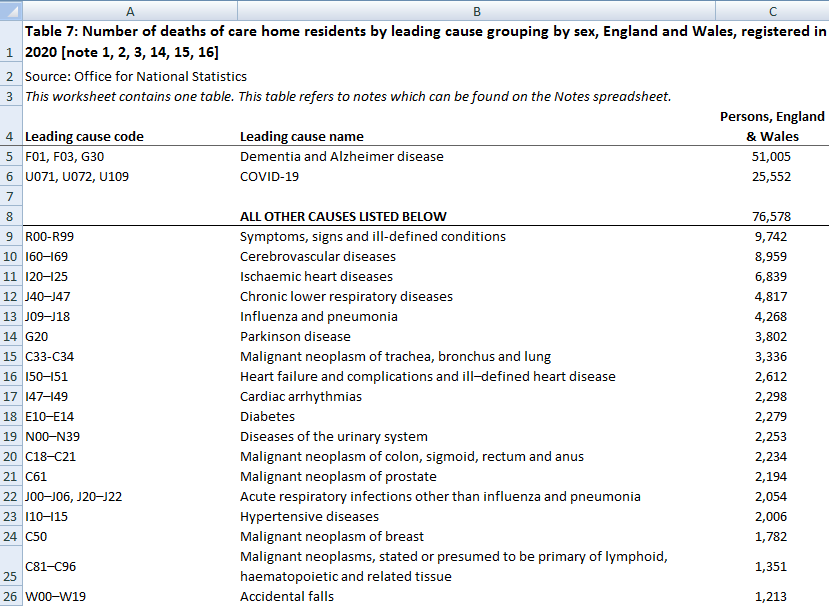
A clue as to what they might have been is provided in tables 7 and 8 of a jolly useful spreadsheet entitled Deaths in the care sector, England and Wales. Table 7: Number of deaths of care home residents by leading cause grouping by sex, England and Wales, registered in 2020 is rather tasty, enabling us to add columns to produce a grand total of persons by leading cause then sorting this by frequency of mention on the death certificate. Here’s a screenshot of my fiddling…
We observe that the leading cause of death throughout 2020 was Dementia and Alzheimer’s disease with 51,005 mentions in total for England & Wales. COVID-19, with it’s extended definition that includes U10.9 (Multisystem inflammatory syndrome associated with COVID-19) comes in second place with 25,552 mentions in section 1 of the death certificate.
Pause For Thought
At this point we need to pause for thought because the definition of what constitutes COVID-19 has changed over time. As the WHO boldly declares, “it all starts with a code”.
At the outset COVID was coded as U07.1 (COVID-19, virus identified) and U07.2 (COVID-19, virus unidentified) but additional codes of U08.9 (Personal history of COVID-19), U09.9 (Post COVID-19 condition) and U10.9 (Multisystem inflammatory syndrome associated with COVID-19) became available to coding authorities from Sep 2020. This extension of the definition means we were counting more cases after Sep 2020 than we were before! Not only that but we were also counting something very different; we may have started out counting incidence of COVID but we ended up counting recovery from COVID as well as incidence. This is a truly excellent lesson on how to cook the books; a lesson brought to us by the chefs at WHO.
It is worth noting that U09.9 and U10.9 are also going to camouflage any and all adverse reactions to the COVID vaccines with overlapping symptomology. Clever, huh?
In Plain English
In plain English it means those 25,552 mentions of COVID in section 1 of the death certificate include a number of cases for whom the virus was never identified and a number of cases who may have been suffering from vaccine injury during Dec 2020 as well as inflammatory conditions not connected to COVID (e.g. autoinflammatory syndrome, chronic inflammatory demyelinating polyneuritis). Thus 25,552 is not exactly a robust number but it does give a ballpark.
All Other Causes
In third place we observe 9,742 certificates with the mention ‘Symptoms, signs and ill-defined conditions’. This is a vague category to say the least and where we’d count people who ‘died of old age’, though I’ve never been sure what that means! If we sum the counts of all other causes we arrive at a total of 76,578 mentions1. The grand total for all causes is thus 153,135 of which COVID-19 represents 16.7% by mention on the death certificate, with Dementia and Alzheimer’s disease representing 33.7%. We thus discover that all other causes represent 50% of mentions between them.
What Does This Mean?
It means that the spike in non-pneumonia deaths during early 2020 is likely to have been a spike in Dementia and Alzheimer’s disease mixed with a variety of other conditions so the issue is rather complex. The statistics tell us something untoward happened that wasn’t connected to COVID or pneumonia that was pretty unique. My money is on iatrogenic causes brought about by dangerous discharge to vacate hospital beds, with the care sector following guidelines instead of questioning matters. Anecdotal evidence coming to me supports this view. If I were to sum everything in one word that word would be panic.
These are not individual deaths since a death may involve more than one cause.


aha! I have a new thought: well not that new at all really, this goes back to my own experience of both hands-on caring for very frail old people, and also managing major institutional closure programmes in the NHS in SE Thames region and Scotland from the mid 1980's onwards...
We know that deaths increased significantly in vulnerable populations of very frail elderly people following the forcible closure of institutions and their transfer to new accommodations. The death rates often doubled for a period of a month or two, then stabilised at porevious rates.
And I can think of at least three possible reasons for this:
a) anxiety and fear - caused by loss of familiar cosy surroundings, loss of personal autonomy, etc
b) loss of continuity of care staff - (who generally had intimate knowledge of the individuals dietary and medical needs)
c) the stress and turmoil of the actual physical move itself
There are some good journal studies about this effect, but I haven't done a literature review or anything like that:
Enforced relocation of older people when Care Homes close: a question of life and death?
https://academic.oup.com/ageing/article/40/5/534/46619
"Abstract
Care Homes are usually seen as the last refuge for older people but residents are sometimes required to move between homes for administrative purposes. There is concern that such moves threaten their well-being and survival. Relocations have been contested repeatedly in court. A recent ruling and its review of case-law and literature provides guidance for practitioners who may be consulted for advice in this demanding situation.
"In spite of public outrage about the quality of institutional care for the elderly and mentally ill in the 1960s, which led to the formation of the Hospital (later Health) Advisory Service [2], further scandals followed. One was at Fairfield Hospital in Bury. Fifteen elderly women with dementia were moved from ward 17 to cold, ill-suited Musberry House at Rossendale General Hospital December 1973. Seven died within the next month and nine within the first 3 months. Only four survived a year [3]. The Bury-Rossendale Inquiry drew attention to the hazards and responsibilities associated with movement of older people for administrative or economic convenience. It concluded prophetically that ‘transfers of groups of patients are likely to become more common, particularly in the fields of psychiatry and geriatrics’."
see also ...
https://voxeu.org/article/rural-hospital-closures-increase-mortality
https://www.nber.org/papers/w26182
https://www.northcarolinahealthnews.org/2019/08/30/closing-rural-hospital-higher-mortality/
I agree with you. Also, my understanding is ... or was until now, untess I can be corrected ... that Dementia and Alzheimer's cannot in and of themselves be a cause of death?