In part 7 of this series I produced a slide of case severity index (CSI) against percentage of staff absences due to COVID that I found perplexing. I had expected the two series to complement each other on grounds that a greater percentage of staff would be going absent during the pandemic peak, which would also be when we’d see elevated levels of case severity1. Against expectation CSI due to COVID and staff illness due to COVID were antagonistic series, causing some readers to speculate on staff absence forcing bed closure. Whilst this is true it misses the point made, so I thought I’d roll out some basic slides that deal with volume and not ratio…
All beds and all absences…
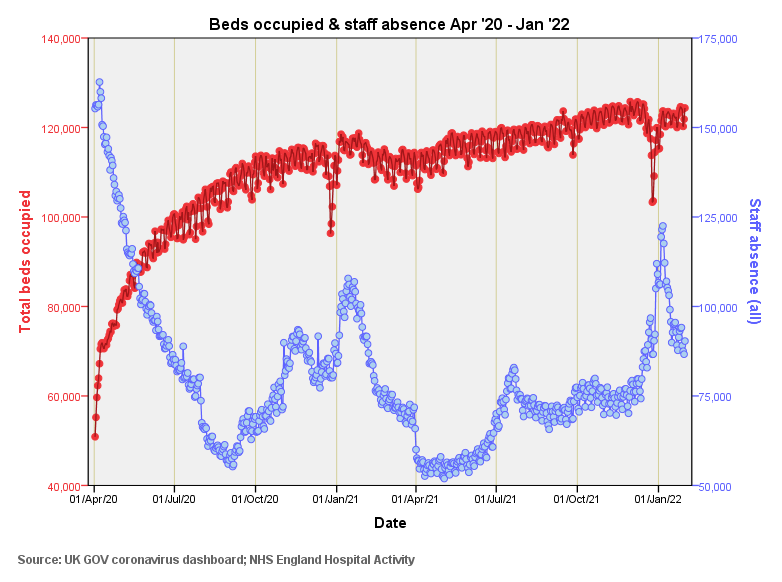
Here is our starting point with everything in the pot. What should be obvious is the strong correspondence between lack of available beds and staff absence back at the beginning of the pandemic. There are two seasonal dips in bed occupancy that correspond to two peaks in staff absence. I wouldn’t pay too much atten…