Do COVID Vaccines Work? (part 12)
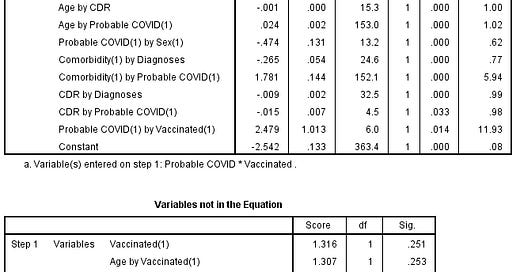
I utilise data from an unknown NHS Trust in the development of a staged multivariate logistic regression model in the prediction of acute respiratory conditions
I left this series hanging in part 11 after being holed below the waterline in my attempt to analyse adult symptomatic COVID in-hospital death over the period 2021/w10 – w37. This aborted attempt followed a suggestion made in part 10, this being:
My next move is to throw away the rather ambiguous meringue of a dependent variable (COVID Dx) and replace it with Symptomatic COVID, then revise the model structure accordingly. To pull in the largest sample possible my definition of symptomatic COVID will simply be any in-patient who received both a positive test result and any respiratory diagnosis prior to death. It will be interesting to see how this simplified approach will swing things.
What all this fiddling boils down to is an attempt to address the diagnostic errors embedded in the EPR, which is supposed to flag genuinely infected and grievously ill COVID cases. Except this WHO-driven approach to diagnosis does nothing of the sort: the indicator variable COVID-19 Dx does not do what i…