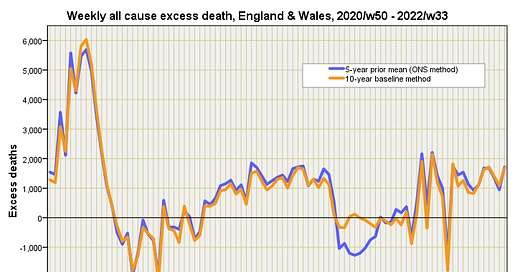
In part 4 of this series I got out the big spanner, this being formal intervention analysis of excess non-COVID death using ARIMA, the idea being to develop a baseline model from which we can ascertain the impact of various independent variables of interest. I waded straight in with case detection rate (CDR) - a proxy for disease prevalence - this being defined as COVID cases per 100 viral tests, which was found to explain around 5% of excess non-COVID death across England & Wales for the period 2020/w50 - 2022/w33 following a 2 week lag. This is an odd finding because disease prevalence shouldn’t figure in a predictive model for non-COVID deaths, and I assumed this may be due to errors with certification.
Then came the big one - vaccination - this being defined as total daily doses of anything they’re jabbing folk with regardless of whether it is first, second or third doses. Unfortunately I was unable to secure fourth and fifth dose data at the time of writing since this data were not presented on the UK GOV coronavirus dashboard. Well, the big one didn’t disappoint with around 30% of excess non-COVID deaths being explained by variation in daily dosing after a 23 week lag… except that model coefficients pointed to vaccine benefit and not harm!
My job now is to try and knock my hypothesis down by expanding my modelling strategy to include the long term impact of lockdown, loss of service provision, long-COVID and deterioration illnesses such as cancer. Meanwhile Joel Smalley, who is about the hottest COVID cruncher out there went, and produced this fine piece of work.